Samenvatting #
Two dogs (Sunny and Bikkel) came to see the ophthalmologist for cataract surgery and are presented in this case discussion. An ophthalmic exam was recommended and, if the patients had no significant problems, a second appointment for cataract work-up and surgery including would follow. Work up includes an ocular ultrasound and an ERG (an electroretinogram, done under anesthesia), immediately followed by bilateral cataract surgery with intraocular lens implantation under the same anesthetic (if bilateral cataract surgery was indicated). The names of the patients have been changed for data protection purposes.
Several points to remember are shown below and are based on several veterinary articles / texts, including:
- Cataract surgery has an excellent prognosis for most animals at approximately 90-95% success. This is granted there are no serious ocular health problems before surgery.
- Vision should be good to excellent after cataract surgery if all is well and a lens implant is used (this is an IOL or intraocular lens implant).
- Cataract surgeons normally choose to place an IOL as this is a ‘gold standard’ of cataract surgery. Although animals can see without an IOL, the IOL restores sight to an optimal degree. The IOL sits inside of the capsule once the cataract has been removed from the lens. Lens luxation cases cannot have an IOL since the capsule is removed with the lens.
- Age is not an impediment for surgery if the general health of the dog is well. Older animals that loose eyesight due to cataracts also experience a significant improvement of quality of life when they can see again.
- Diabetics are a special group. Diabetic cataracts can cause blindness very quickly because they can mature (i.e. become white) very quickly. It should not surprise us that owners report the animal “could see yesterday (or last week) and can no longer see since today”.
- Also, 50% of diabetic dogs develop cataracts 170 days after diagnosis of diabetes and this number increased to 75% by 370 days and 80% by 470 days (in one large study). This means diabetic cataracts are very common in diabetic dogs and should be expected in 75% of cases in about 1 year since diagnosis of diabetes. However, at least 50% of diabetic dogs will develop cataracts within about 5 months.
- Diabetic cataract surgery also has a good prognosis. However, diabetic cataracts absorb a lot of water and quickly swell up. This can lead to ‘spontaneous lens rupture’ and this is why we like to operate diabetics with cataracts as soon as possible (i.e. before they rupture).
- Spontaneous lens rupture in diabetics is not common, but it is a severe complication. Therefore, it is better never to wait for good glycemic control to refer a diabetic for cataract surgery and to let the referral center know that the patient is a diabetic so that surgery can be carried out as soon as possible.
Further reading (enter the title of the article in www.pubmed.com to read the abstract):
Beam S, Correa MT, Davidson MG. A retrospective-cohort study on the development of cataracts in dogs with diabetes mellitus: 200 cases. Veterinary Ophthalmology. 1999; 2(3): 169-172.
Wilkie D. and Colitz C. Surgery of the lens (Ch 22). In: Veterinary Ophthalmology. Gelatt, Gilger and Kern editors. 5th Edition. Wiley-Blackwell. p2013: Pg. 1234.
Wilkie DA, Gemensky-Metzler AJ, Colitz CM, Bras ID, Kuonen VJ, Norris KN, Basham CR. Canine cataracts, diabetes mellitus and spontaneous lens capsule rupture: a retrospective study of 18 dogs. Veterinary Ophthalmology. 2006; 9(5): 328-334.
R. F. Sanchez. Staar bij honden. Is chirurgisch vaak goed te verhelpen. Onze Hond. 2020; 6 (juli): 96-99. (not available through PubMed).
Behandelend arts #
Rick F. Sanchez, BSciBiol, DVM, CertVOphthal, DipECVO, FHEA
EBVS accredited, European Specialist in Veterinary Ophthalmology
Patiënt #
Sunny (dog1): Weimaraner, male neutered, 3 years old
Bikkel (dog2): Labrador, male non-castrated, 6 years old
Anamnese #
Sunny (dog1): he had deteriorating vision and was unable to see well at night. The patient became less comfortable and less sure of himself, and the owners wanted to find out if the problem were cataracts or something else, and if they could do something about it to improve his life. He was found to be a perfect candidate for cataract surgery.
Bikkel (dog2): he was a diabetic and he quickly developed cataracts and the eyes were a little red. The owners and the veterinarian were worried about glucose control and focused on that aspect of his illness first, so Bikkel was not referred for cataract surgery for 2 months. Unfortunately, he developed bilateral spontaneous lens rupture, intraocular bleeding and massive ‘phacoclastic’ uveitis, all of which ultimately led to retinal detachment and permanent loss of vision. Surgery could not help him. A terribly sad situation that is uncommon but that highlights the importance of always operating diabetic cataracts with urgency, as soon as possible, just in case.
Beeldvorming #
The preoperative ultrasound examination is performed by one of our radiologists, nearly always in the presence of the ophthalmologist.

Figure 1 shows the ultrasound image of a healthy canine lens in a healthy canine eye.

Figure 2 shows a mature diabetic canine lens that has absorbed water and is enlarged. The volume the lens occupies is much larger than in Figure 1.


Figure 3 and 4 show a bilateral ruptured right and left lens of a diabetic patient with cataracts. This patient also had blood in the eye and a severe uveitis, which unfortunately meant his prognosis was very poor. His lenses ruptured 2 months after the diagnosis of diabetes.
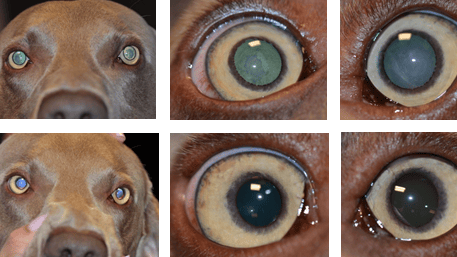
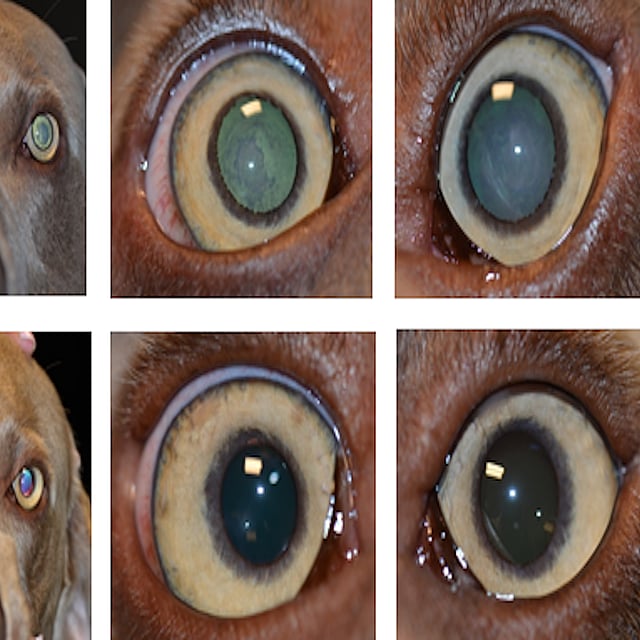
These images show the patient before (above) and after (below) cataract surgery. The pupils look gray and although they are not mature cataracts (they are not completely white yet) the cataracts are interfering with vision to a significant degree. The patient had bilateral cataract surgery with IOLs and did very well.

Image of the ERG (electroretinogram) of a working / healthy, canine retina. We expect to see a wave of a total amplitude of 80+ microvolts (in this case the amplitude was just over 100 microvolts when adding the negative -50 and positive +50 - we do not take the signs into account, or it would otherwise add to zero). There Is a downward wave (‘a’ wave) followed by a quick upward wave (‘b’ wave) with small wavelets in it that has a gentle downward slope (this later leads to a ‘c; wave). The waves correspond to electrical current being generated in response to a light stimulus and then carried throughout the retina.
Bevindingen #
The significant findings of the ophthalmic exam for each patient included the following:
Sunny (Dog1): Immature bilateral cataracts. Mild lens induced uveitis seen with normotensive eyes (12mmHg in each eye with rebound tonometry (ref 12-24mmHg)) and normal tear production (STT 18mm/minute in each eye (ref. ≥15mm/min in the absence of pain) and no other problems to report. The fundus could still be observed but an ocular ultrasound and ERG were performed. The ultrasound found no problems and the ERG was suggestive of a working retina.
Bikkel (Dog2): Mature cataracts with severe lens induced uveitis. Suspected bleeding inside of each eye and possible spontaneous lens rupture. An ocular ultrasound confirmed the presence of ruptured lenses.
Diagnose #
Bilateral cataracts in both cases. The diabetic patient was also diagnosed with spontaneous lens rupture with bleeding in the eye and acute, severe phacoclastic uveitis and bleeding in the eyes.
Behandeling & therapie #
Since the prognosis for cataract surgery is excellent (around 90-95% of cases do very well with careful patient selection, pre-surgery work-up and careful follow up and monitoring in the case of dogs, and slightly less, about 90% to 93% for rabbits and cats, respectively), surgery was recommended and expected to have a good prognosis for Sunny. Unfortunately, sight could not be restored for Bikkel, the patient with spontaneous lens rupture, who was given a guarded-to-poor prognosis. Early referral for diabetic patients is recommended.
Post-operative therapy for cataract cases includes drops (this is normally only an antiinflammatory drop that is tapered off over a period of 4 weeks and then it is used 1x day or once every other day for life, although sometimes a drop to help control the eye pressure is also used), a collar that protects the eye for 2 weeks and then can be removed, and an oral antiinflammatory medication that is used for the first 4 weeks after surgery.
At the SDU, to obtain the best results possible, cataract surgery patients are monitored closely the first night with a veterinary professional that stays in the hospital overnight to measure the eye pressure and monitor the patient for the first 24 hours after surgery. This is followed by very carefully monitoring overtime (i.e. usually 4 re-examinations in the first year after surgery, and then 1 examination once per year for the rest of the animal’s life independent of the species /breed).
The author retains all intellectual property rights of this article, including the text and images. The content of the article and its parts may not be reproduced or reused without specific permission from the author.